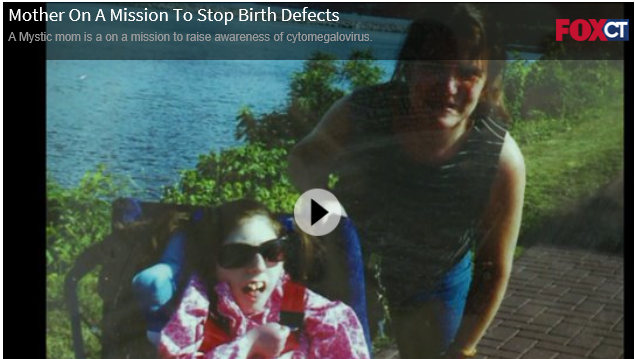

Lisa Saunders Press Release (CMV)
Listen to the Centers for Disease Control and Prevention's Podcasts, Staying Healthy When a Baby's on the Way:
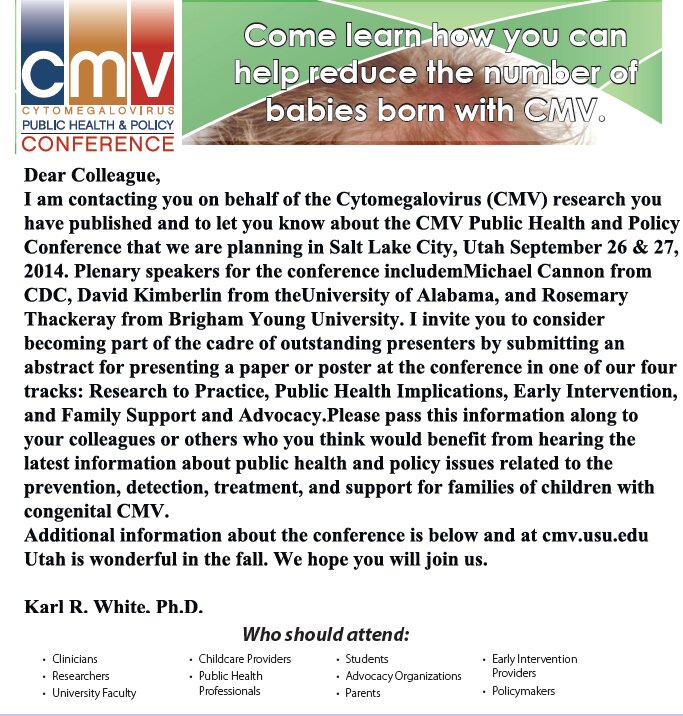
What is Cytomegalovirus (CMV)
CMV, or cytomegalovirus (si-to-MEG-alovi-rus), is a common virus that infects people of all ages. Most infections with CMV are “silent,” meaning most people who are infected with CMV have no signs or symptoms. However, CMV can cause disease in unborn babies and in people with weakened immune systems. Once CMV is in a person's body, it stays for life. The mission of the Congenital CMV Foundation is to prevent birth defects resulting from congenital CMV infection.